
Not too long ago, healthcare was all about personal connections between doctors and patients, using handwritten notes and talking directly. But as healthcare grew and more information about patients came in, it became clear that we needed a better and more organized way of doing things. Hospitals and clinics had to change how they worked, aiming for smoother processes, quicker decision-making, and better communication among healthcare workers.
To tackle challenges like common capacity and operational issues, Healthcare Command Centers (HCCs) were introduced. Now, don’t picture it as some high-tech, dimly lit room with specialists surrounded by giant monitors. Hospital command centers are less dramatic, they function as centralized hubs where various healthcare data is efficiently managed, helping hospitals streamline operations, enhance coordination, and improve overall patient care.
If you want to learn more about what HCC does then continue reading this article to discover how it tackles existing problems in healthcare management and the practical benefits it brings to healthcare organizations (HCOs).
The Role of Healthcare Command Centers
A healthcare command center is like the smart control center for hospitals, where they coordinate everything related to patients. Instead of having different departments working separately, like transfers, bed management, transport, and patient access, the command center brings them all together. This can be done physically, virtually, or a mix of both.
The main job of the command center is to actively manage how patients move through the hospital and handle related services. They use real-time data and analytics to make decisions on the spot. The ultimate goal is to improve communication, keep an eye on what's happening with patients, and make decisions based on that information. Depending on the organization, these command centers can focus on one hospital, multiple hospitals, or even the entire healthcare system.
In the last five years, some hospitals in different countries have been even trying out these command centers to manage how patients move through the hospital. The results so far are promising. For example, at Johns Hopkins Hospital in the USA, transferring patients from other hospitals got 46% better, ambulances arrived faster by 43 minutes, and emergency patients got their beds 3.5 hours quicker.
Components of a Healthcare Command Center
A healthcare command center works well when it brings together different parts smoothly.
1) Technology Foundation: At the heart of any HCC is a strong technology base. This includes good-quality equipment, software, and networks. These help handle, understand, and show a lot of healthcare information in real-time.
2) Data Analysis: It's important to be able to look at both old and current data. HCCs use smart tools to find patterns, guess how patients will move, and figure out possible problems. This helps make decisions before issues happen.
3) Communication: HCCs need to help different parts of a hospital talk to each other easily. This involves using communication channels that are joined together. This way, important information can be quickly shared.
Integration with Existing Healthcare Systems
Working with Existing Systems: To work well, HCCs need to fit with the systems hospitals already have. This includes things like Electronic Health Records (EHR), Clinical Decision Support Systems (CDSS), data storage and analysis tools, and payment systems. By connecting with these, HCCs make sure information moves smoothly, reducing repeated work and making the healthcare system work together better. Cooperation with other parts of the hospital, like emergency services, tests, and patient care units, is also important. This helps everyone work together for better healthcare.
How Healthcare Command Center Works?
Let's talk about how a Healthcare Command Center usually works:
1. Collecting Information
To start, we gather all sorts of important and up-to-date data from different healthcare sources. This includes things like real-time patient details, electronic health records, admission and discharge records, and info from monitoring systems. This helps us have a varied and current set of data.
2. Sorting Out the Data
After getting the data, we clean it up to make sure it's accurate and consistent for good analysis. Think of it as tidying up the information, making it all standard, and putting it together. This step ensures that when we analyze the data, we're working with trustworthy and uniform information.
3. Making Data Easy to Understand
Once the data is cleaned up, we turn it into a visual form that's easy to grasp, like charts and dashboards. These visuals give a clear picture of things like how patients are moving through, how resources are being used, and other important facts. They're like shortcuts for healthcare professionals to quickly get what's going on.
4. Figuring Things Out from the Data
Now comes the part where we dig into the processed data to find meaningful insights and understand patterns. We use some advanced techniques like statistical modeling and machine learning. For example, we might look at past patient admission data to predict what might happen in the future. This helps us plan ahead, like deciding how to allocate resources and staff.
5. Supporting Decision-Making
Based on what we find, the command center helps with decision-making. This means using the insights to make choices about things like where to put resources, adjusting staffing levels, and responding to emergencies. The goal is to make healthcare delivery more efficient and improve how patients are taken care of.
These steps all fit together like a loop, letting the healthcare system adapt, learn from past data, and keep getting better. The command center's job is to handle current situations while using what it learned from the past to make healthcare operations better over time.
Nonetheless, the future of healthcare is fueled by data. On average, a hospital generates 50 petabytes of data each year—enough to fill about 500 billion pages of printed text. Despite this staggering volume, 97% of this data goes unused due to silos and lack of standardization. If you want to know more then listen to our podcast to learn about leveraging interoperability for effective healthcare management.
How Can Hospitals Make the Most of Healthcare Command Centers?
Hospitals are finding new ways to enhance their operations and improve patient care through healthcare command centers. Let's explore some practical ways hospitals can use these command centers to boost efficiency and responsiveness in today's ever-changing healthcare landscape.
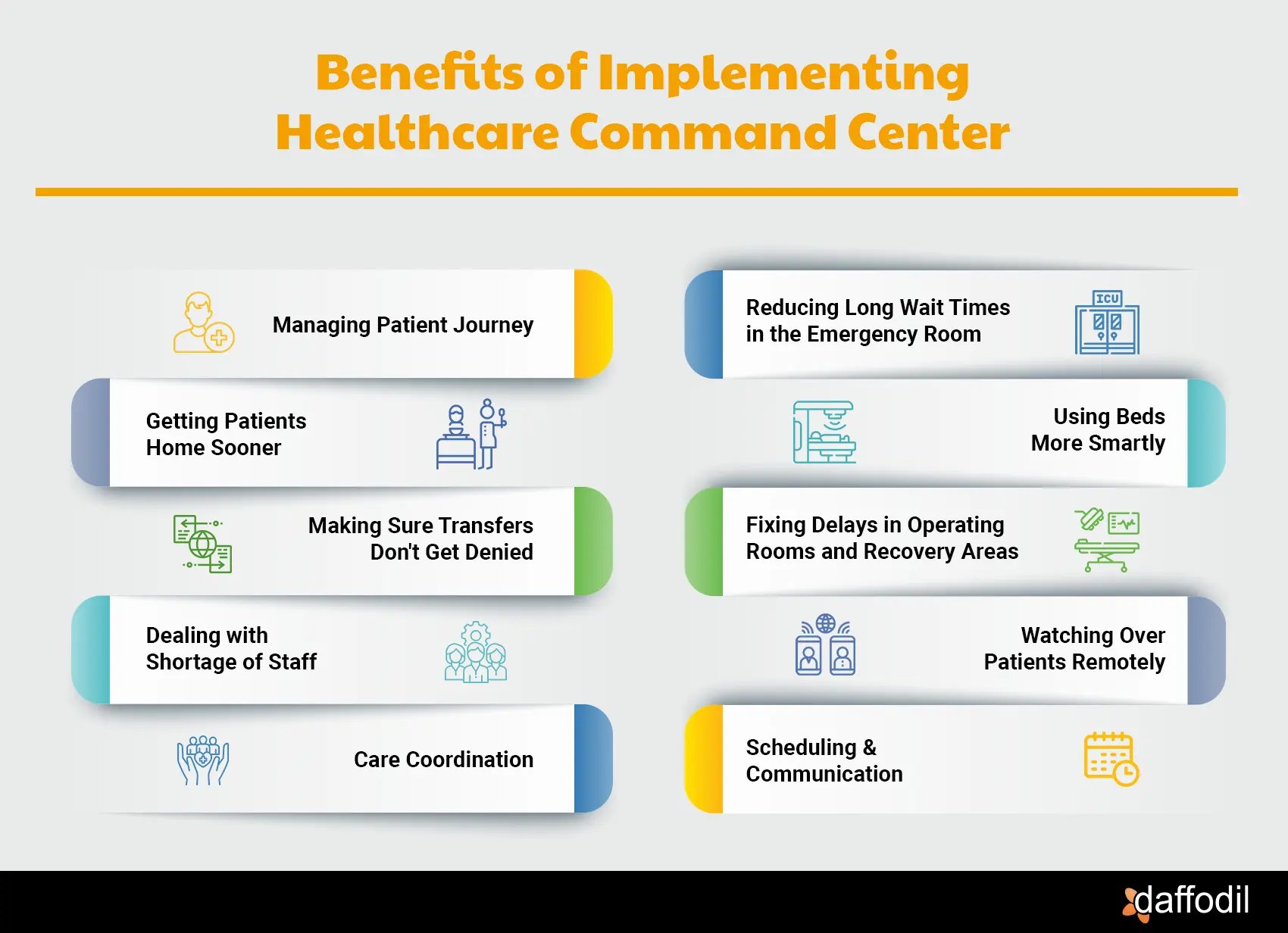
1) Managing Patient Journey: Beyond just keeping tabs on patients in real-time, command centers give a complete picture of patient journeys within the hospital. This helps hospitals ensure timely care and identify areas where processes can be streamlined. Hospitals can regularly evaluate their performance by keeping an eye on metrics like how long patients stay, the availability of beds, and other key indicators to continually refine their operational strategies.
2) Reducing Long Wait Times in the Emergency Room: HCCs help hospitals deal with the problem of patients waiting too long in the Emergency Department (ED) for a bed. This waiting can cause overcrowding, safety issues, and harm to patients. The HCC keeps an eye on how many patients are waiting and how long they've been waiting, allowing hospital staff to make quick decisions to improve the situation. They can also activate special plans, like redirecting ambulances or getting patients out of the ED faster.
3) Getting Patients Home Sooner: Sometimes, patients end up staying in the hospital longer than expected, which can cause problems. HCCs help hospitals look at the whole journey a patient takes from when they arrive to when they leave. By doing this, they can make decisions that help patients get home faster. This not only improves the time people spend in the ED but also gets them into a regular hospital bed more quickly.
4) Using Beds More Smartly: In some hospitals, there might be too many patients needing beds, and not all of them need the same level of care. HCCs help hospital leaders see the bigger picture of bed availability. This way, they can move patients around more efficiently, making sure each patient is in the right kind of bed and not waiting unnecessarily.
5) Making Sure Transfers Don't Get Denied: Hospitals sometimes have to say no to transferring patients from one place to another because there aren't enough beds. This can be a big problem for patient care and also for the hospital's finances. HCCs help hospitals balance how many beds they have inside with how many patients need to come in from other places. This way, they can say yes to more transfers and keep things running smoothly.
6) Fixing Delays in Operating Rooms and Recovery Areas: If patients have to wait too long in the operating room or recovery area, it can be costly and disrupt the schedule. HCCs keep an eye on delays in real-time and over time, so hospital staff can make changes to schedules, move patients around, or even get patients to a different kind of care area to avoid unnecessary waiting.
7) Dealing with Shortage of Staff: Getting the right staff to the right place in a hospital can be tough, especially when there aren't enough people to go around. HCCs keep track of where there are gaps in staffing and try to move existing staff to the areas that need them the most. It's not a perfect solution, but it helps hospitals manage with the people they have.
8) Watching Over Patients Remotely: HCCs also help smaller hospitals keep an eye on patients using remote monitoring. This could be things like watching for falls through video cameras or keeping an eye on patients for signs of infections. This helps smaller hospitals provide better care without needing as many staff or resources.
9) Care Coordination: By incorporating simple metrics like patient satisfaction and response times, hospitals can assess and improve how well teams work together. Automatic alerts can help hospitals notify healthcare providers promptly about important events. This ensures teams can respond swiftly to changes in a patient's condition, potentially preventing complications and improving overall patient outcomes.
10) Scheduling & Communication: Command centers play a role in automating the scheduling of appointments, procedures, and resource use. This simplifies operations and improves scheduling accuracy. By providing a shared communication platform, command centers promote collaboration among staff from different departments. This reduces delays, allowing the hospital to respond more efficiently to emerging situations.
Why HCOs Should Consider Healthcare Command Centers
Investing in a healthcare command center can bring many advantages to hospitals and improve healthcare services. Here are nine reasons why it's a good idea:

1) Savings on Costs: By using HCC, hospitals can save money over time. It helps them use resources more efficiently, cutting down on unnecessary expenses.
2) Adaptability: HCC is made to adapt easily to the changing needs of healthcare systems globally. It's cost-effective, allowing healthcare facilities to grow and improve without spending too much.
3) Easy Integration of Patient Data: HCC makes it simple to combine different types of patient information from various sources. This makes decision-making more informed and helps create a unified view of patient data.
4) Customization for Local Needs: Hospitals can easily customize HCC to fit local languages, practices, and regulations. This makes it more effective and relevant in different healthcare settings.
5) Remote Monitoring: With command centers, hospitals can monitor patients remotely. This extends the reach of healthcare services, especially important in urgent situations, leading to better patient outcomes.
6) Efficient Operations: Optimizing resources means using staff, equipment, and facilities more effectively. Command centers help different hospital departments work together better, reducing delays and improving workflows.
7) Strong Security and Compliance: HCC prioritizes strong security measures, making sure hospitals comply with data protection rules. This builds trust among patients and healthcare professionals.
8) User-Friendly Design: HCC is designed with users in mind, making it accessible for healthcare professionals at all levels of the workflow.
9) Reliability and Less Downtime: HCC is built to be highly reliable, with backup solutions to ensure operations continue smoothly. This is crucial for maintaining healthcare services without interruptions, especially in critical situations.
How to Get Started With Healthcare Command Centers
Starting with HCCs involves assembling a team that wears different hats – a mix of folks from various departments. Think of it like putting together a band with diverse talents. These team members will help set the goals for the command center, figuring out what it should achieve.
Next, spot the bumps in the road. What are the challenges that could slow things down? Pin them on your defined roadmap and decide which ones to tackle first. Be crystal clear about what success looks like. Set goals that are like signposts, showing you're on the right track. Measure everything, so you know you're headed in the right direction.
If you're looking for an expert HealthIT team to transform your healthcare operations, then partner with Daffodil. Our seasoned experts ensure a tailored strategy, seamless integration, and effective governance. Partnering with us guarantees a sophisticated and efficient HCC tailored to your institution's unique needs, ensuring optimal patient care and operational excellence from day one.







