In recent times, the way healthcare works has changed significantly. Instead of solely relying on traditional methods such as paper records and telephone communication, the integration of software and digital technology has brought about a complete transformation in the delivery of healthcare services.
Why did this change happen? Well, healthcare needed to be faster, more accurate, and easier to use. Today, software plays a pivotal role in various aspects of healthcare, such as electronic health records (EHR) management, telemedicine, diagnostic tools, remote patient monitoring tools, and more. These digital solutions not only facilitate seamless communication among medical professionals but also empower patients to take control of their health through online portals and mobile applications.
However, healthcare providers often face a challenge. It's about figuring out how to use software in the right way for healthcare. To make the most of healthcare software, you need to understand how it's put together – the software architecture. Making sure this internal structure is well-planned is really important for the software to work smoothly with the existing healthcare systems.
In this blog, we'll explore the key factors that should guide your choices when designing healthcare software. Additionally, we'll cover an example of telemedicine app architecture and discuss its various components.
What are the Key Factors that Impact Healthcare Software Architecture?
1. Understanding your healthcare goals: Just as blueprints guide the construction of a building, your software architecture must align with your healthcare organization's strategic goals. Consider whether the architecture will support telemedicine services, electronic health records (EHR) management, or medical imaging solutions. This alignment ensures that the architecture serves the purpose of your healthcare services.
2. Data Elasticity: Healthcare deals with vast amounts of data, so your software architecture needs to scale seamlessly. It must handle growing patient data volumes and user loads without compromising performance. Opt for an architecture that supports horizontal scaling, allowing you to add more servers or resources as needed.
3. Interoperability: Your software architecture should easily integrate with the broader healthcare ecosystem. This includes interfacing with EHR systems, laboratory information systems (LIS), picture archiving and communication systems (PACS), and other relevant platforms. An architecture with well-defined APIs and standard communication protocols promotes interoperability.
4. Security and Compliance: Just as businesses prioritize data protection, your software architecture must be secure and comply with healthcare regulations like HIPAA and GDPR. Patient data security is vital, and your architecture should ensure proper data encryption, access controls, and audit trails.
5. Microservices Modularity: As more people adopt your healthcare software, you might consider adding extra features to match the growing demand. This is when you need to make sure that your software's inner structure can handle all the extra users and work. Using a microservices architecture enhances software development agility. So, break down complex functionalities into smaller, self-contained microservices. This modularity enables rapid feature development, easier maintenance, and seamless scalability of specific components.
6. User-Centric Interface: Similar to a building's layout for optimal functionality, you must prioritize user-centered design in your architecture. Whether it's clinicians, administrative staff, or patients, a well-designed architecture should support an intuitive interface and efficient workflows.
7. Performance Optimization: Healthcare software's responsiveness is vital, especially in critical situations. Your architecture must efficiently process data and swiftly respond to user actions. Utilize strategies like caching mechanisms, load balancing, and content delivery networks to minimize response times and ensure smooth user experiences.
8. Deployment Flexibility: Deployment flexibility allows healthcare organizations to adapt their software to their unique operational needs while ensuring data security, regulatory compliance, and optimal performance. It empowers you to make strategic choices based on factors like cost, data sensitivity, and technical requirements, ultimately leading to a more tailored and effective healthcare software solution.
For instance, a telemedicine application might benefit from cloud scalability to handle varying patient loads. On the other hand, a hospital might prefer on-premises deployment to ensure full control over patient data. Therefore, your architecture should seamlessly integrate with the chosen deployment model.
READ MORE: 5 Commonly Used Cloud Deployment Models
9. Technology Stack Selection: Your software architecture relies on a technology stack. Therefore, ensure your chosen stack aligns with healthcare software development best practices, taking into account the programming languages, frameworks, and tools commonly used in the industry.
10. Budget Constraints: Evaluate the budget available for your software project. Different architectures come with varying costs, so align your choice with your financial resources.
11. Consulting Industry Experts: Just as architects consult structural engineers, seek advice from experienced healthcare software architects. Collaborate with professionals who possess domain-specific knowledge and have successfully designed healthcare systems. These experts can provide insights into architectural patterns, best practices, and potential pitfalls specific to healthcare software.
Let’s understand more with an example of telemedicine app architecture:
The architecture of a telemedicine system can be categorized into four key segments: users, communication elements, APIs and operational logic, and data storage.
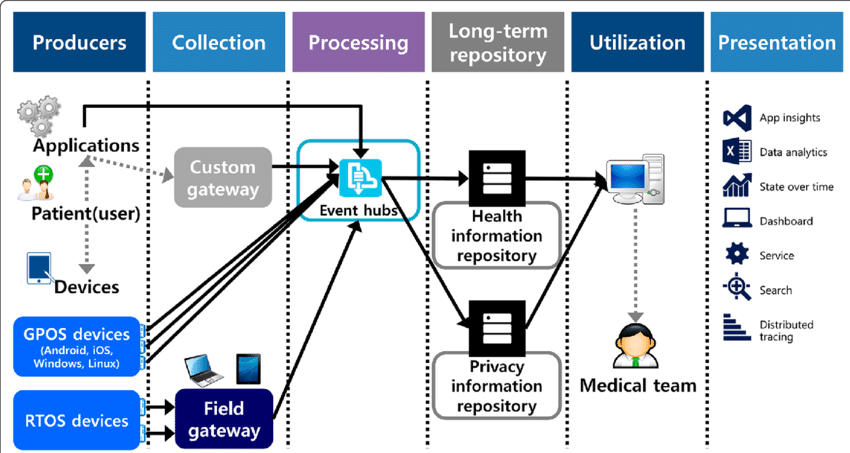
Image source: ResearchGate
1. Client
A client is like a face or a tool that users interact with. In the case of a telemedicine platform,
There are three different groups of users—patients, doctors, and administrators.
These clients can come in the form of mobile apps for smartphones or web portals that you access through computers. The choice of technology for building these clients depends on whether you prefer mobile apps, web-based platforms, or a mix of both, depending on your platform's goals and what users prefer.
2. Effective Communication
Effective real-time communication is the cornerstone of a telehealth platform, facilitating essential interactions between patients and practitioners. This interaction can occur through video streaming, live chat, audio, or a combination of these methods.
Choosing the right communication channels is crucial, and many existing platforms incorporate both video streaming and live chat capabilities.
Now, what sets telehealth apps apart from regular chat apps is the imperative need for HIPAA compliance. This refers to a set of rules that ensure patient information remains confidential. As any conversation between patients and doctors involves private health details, it all falls within these rules. However, ensuring top-notch security can be complex.
The Health Insurance Portability and Accountability Act (HIPAA) is a federal law designed to safeguard sensitive patient health information from unauthorized disclosure. Violations of HIPAA regulations can result in significant penalties, starting from a minimum fine of $50,000 for willful violations.
Fortunately, there's no need to undertake this cumbersome process independently. Daffodil offers cloud-based HIPAA-compliant software solutions that are not only easy to configure but also seamlessly integrate with any existing system. This alleviates the burden of establishing and maintaining robust security measures, enabling healthcare organizations to focus on delivering high-quality telehealth services while ensuring the protection of patient data and adhering to legal standards.
3. APIs and Business Logic Layer
In the telehealth arena, different players need to talk to each other smoothly. These players include clients, databases, and external software. Making this happen involves using APIs (like connectors) and business logic.
To make this effectively work, microservices come into play. These microservices have specific roles and operate on computing systems such as AWS or Azure.
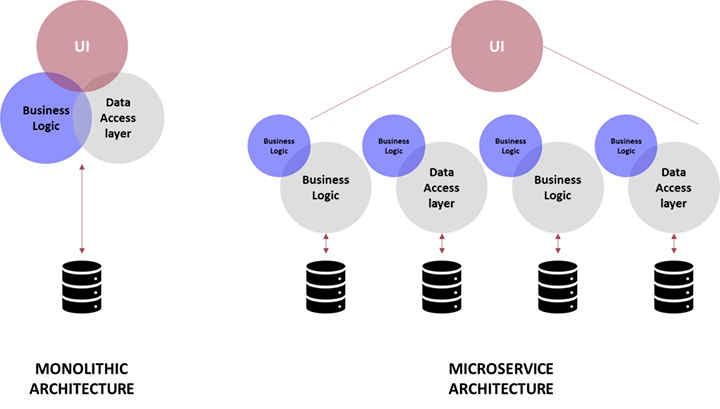
Image source: Sterling
Each microservice has its own task. Some handle video calls, while others ensure secure logins in the web portals. They can even facilitate the direct sharing of health data from wearable devices like Apple Watches to your doctor or your medical records. This streamlined approach expedites the development of a telehealth app by leveraging pre-built tools.
Now, the important part is the business logic layer. It's like the manager of communication between clients and the server. It's also the brain behind "operational logic" which decides how data is changed, counted, stored, and shared. This includes tasks such as providing guidance, ensuring secure logins, and maintaining organized data for quick access.
4. Data Storage
Another critical aspect of how a telemedicine system operates involves managing data effectively and setting up the necessary technical framework. Cloud-based services such as AWS, Azure, or Google Cloud are often employed for this purpose. These services act as virtual storage spaces where the telemedicine system keeps its data in order.
The cloud service takes on important responsibilities, such as managing the part of the system that allows different parts to communicate, load balancing, CDNs (Content Delivery Networks), and version deployments.
When creating a telemedicine system, it's crucial to pick a cloud service that complies with HIPAA regulations. This is because the system will hold private health information in its databases. AWS and Azure are popular choices because they have strong security measures in line with HIPAA requirements.
How Daffodil Software Helped a US-based Health Tech Firm Build an AI-powered Telehealth Platform?
In the complex healthcare landscape, addressing the shortage of healthcare professionals and reducing wait times for appointments has been a significant challenge. However, MayaMD is reshaping the healthcare landscape with its innovative solution: an AI-powered chatbot called Maya, combined with a robust telehealth platform.
MayaMD's primary focus is to make healthcare more accessible and convenient. To accomplish this goal, MayaMD has collaborated with our team of experienced AI experts to develop a user-friendly mobile app. This app offers patients personalized treatment recommendations, fundamentally transforming the way healthcare is delivered.
At the core of the mobile app is an AI-powered symptom tracker. This feature empowers patients, Maya, and physicians to analyze health concerns based on selected symptoms. The mobile app acts as an essential tool, conducting comprehensive symptom assessments through the MayaMD AI engine on behalf of patients. Physicians can access their patient list, monitor vital signs, review symptom tracker notes, start video calls, set appointments, and do more.
This platform also offers a range of features to patients. They can request appointments, stay on track with medications, refill prescriptions, access billing & compliance reports, set reminders and tasks, and more. The app empowers patients to take an active role in managing their healthcare.
The development of MayaMD's chatbot was made possible through the utilization of cloud computing resources. By harnessing the scalability, computing power, and flexibility of the cloud, MayaMD's chatbot can easily interact with patients and provide immediate assistance for their health concerns. Cloud computing enables the chatbot to process vast amounts of data, analyze patient information, and deliver personalized recommendations, ultimately improving health outcomes and enhancing the quality of life for patients.
Read the full case study here.
Select the Right Software Architecture for Improved Healthcare Delivery
Just as medical treatments improve over time, the way we build software also keeps getting better. Software architecture plays a leading role in this progress. It drives new ideas, helps patients get better care, and shapes how we experience healthcare in exciting new ways.
Still struggling to structure your healthcare software? Look no further—our healthcare IT experts are here to assist. With over 20 years of experience as a leading healthcare software development company, our seasoned professionals thoroughly examine your needs. They develop personalized solutions that seamlessly integrate into your operations. Partner with us to enhance your healthcare delivery using robust software architecture.
Ready to take the first step? Book a free consultation with us!






